Introduction
Clinical research is undergoing a fundamental shift. Decentralized and AI-augmented clinical trials (DCTs) are redefining how pharmaceutical studies are designed, conducted, and analyzed by moving away from traditional site-centric models toward patient-centric, digitally enabled trial ecosystems. Accelerated during the COVID-19 pandemic, these approaches demonstrated that robust clinical evidence can be generated remotely while maintaining scientific and regulatory standards (Dorsey & Topol, 2020).

What Are Decentralized Clinical Trials?
Decentralized clinical trials are studies in which some or all trial activities are conducted outside conventional investigator sites, often in participants’ homes. Digital technologies enable remote recruitment, consent, monitoring, and follow-up. Based on the degree of decentralization, DCTs are broadly categorized into:
Fully decentralized (virtual) trials
Hybrid trials combining on-site and remote activities
Site-supported remote trials
Among these, hybrid models are most widely adopted due to their balance between flexibility and regulatory feasibility (Unger et al., 2023).

Key Components of Decentralized Trials
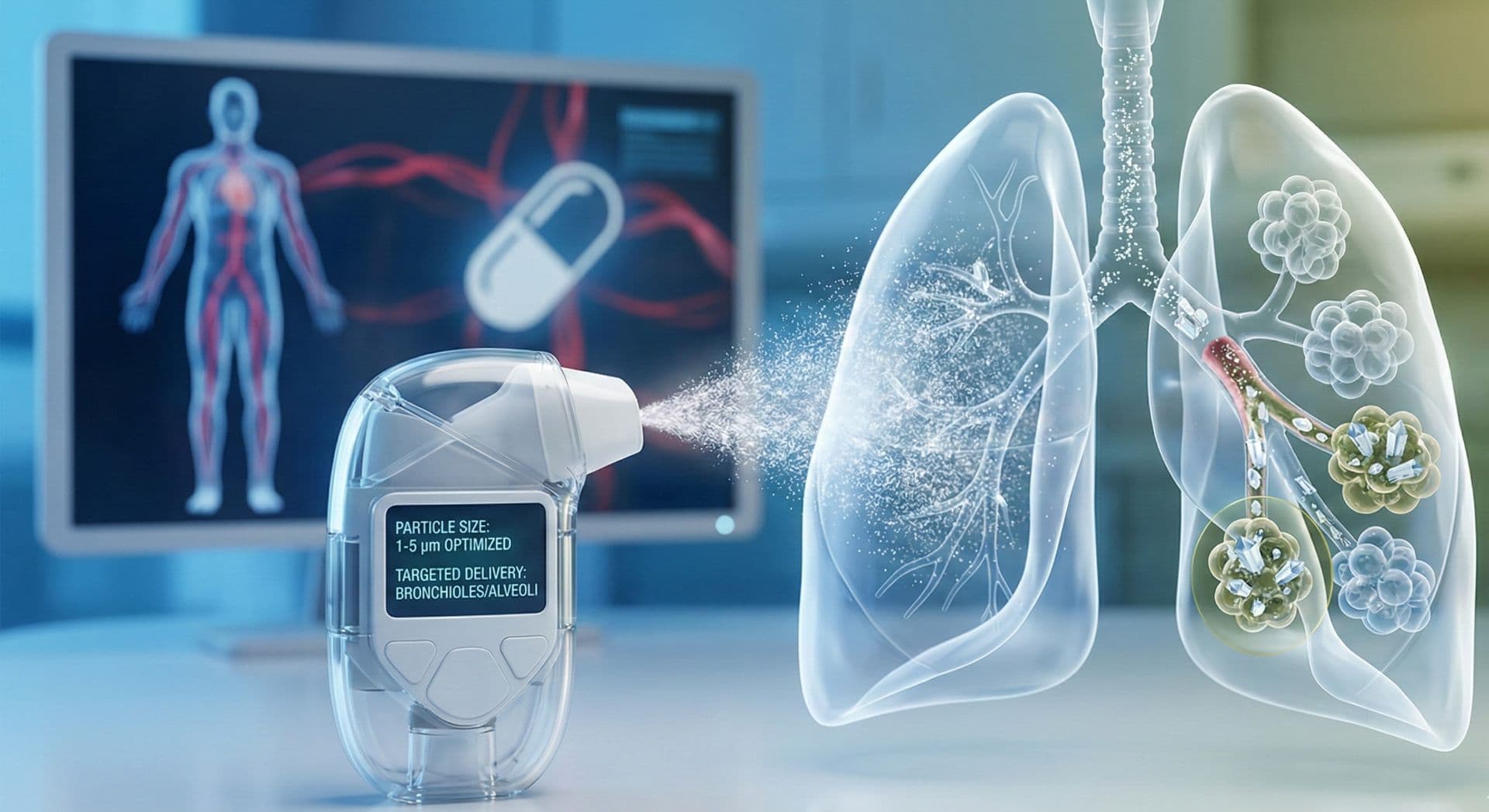
DCTs rely on an integrated digital infrastructure that supports trial continuity outside physical sites. Core components include telemedicine visits, electronic informed consent (eConsent), wearable sensors, electronic patient-reported outcomes (ePROs), home nursing services, and direct-to-patient delivery of investigational products. These elements reduce participant burden, improve retention, and enable continuous data collection, particularly valuable for chronic and rare disease studies (Califf & Hernandez, 2021).
Role of Artificial Intelligence in Clinical Trials
Artificial intelligence enhances decentralized trials by transforming large volumes of digital data into actionable insights. AI is used for predictive patient identification, enrollment optimization, adaptive protocol design, automated data cleaning, medical coding, and real-time safety monitoring. Machine-learning algorithms also support risk-based monitoring and early detection of protocol deviations, improving trial efficiency and data quality (Topol, 2019; Bender & Beckmann, 2021).

Why Decentralized and AI-Augmented Trials Matter
The combined use of decentralization and AI offers significant scientific and operational advantages. These include faster recruitment, broader demographic representation, improved patient engagement, reduced operational costs, and shortened development timelines. Continuous digital data streams also support real-world evidence generation, strengthening regulatory submissions and post-marketing evaluations (Unger et al., 2023).
Regulatory and Ethical Considerations
Regulatory authorities increasingly accept decentralized trial elements when aligned with Good Clinical Practice, data integrity, and patient safety requirements. However, challenges persist, including data privacy, algorithm transparency, digital inequity, device validation, and interoperability across digital platforms. Addressing these issues through robust governance frameworks and ethical oversight is essential for sustainable implementation (Vayena et al., 2021).
Future Outlook
Decentralized and AI-augmented clinical trials are no longer experimental innovations but strategic imperatives in modern pharmaceutical research. As digital health technologies mature and regulatory clarity increases, these models will continue to accelerate drug development, enhance patient participation, and improve the overall quality of clinical evidence (Dorsey & Topol, 2020).